Prevent Achilles Injuries: Tips for Athletes
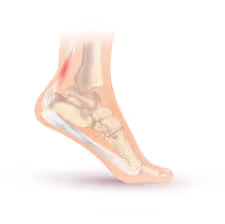
The Wilmington community thrives on an active lifestyle. From the sandy shores where runners hit their stride, to the vibrant courts filled with pickleball and volleyball enthusiasts, and the fields where soccer and basketball reign supreme, our community is a hub of athletic energy. For many, the biggest fear isn't a shark lurking in the surf or an alligator by the Intracoastal, but rather the abrupt, career-altering pop of an Achilles tendon. This vital band of tissue, connecting your calf muscles to your heel bone, is paramount for the explosive movements these beloved sports demand. When an Achilles injury strikes, it can derail not only athletic pursuits but also daily life, leaving individuals sidelined and frustrated. Understanding these injuries, how they occur, and the most effective strategies for recovery and prevention is crucial for anyone looking to maintain an active lifestyle in our dynamic coastal city.
The Grades of Achilles Strain: A Spectrum of Severity
Achilles injuries often fall under the umbrella of strains or tendinopathies, varying in severity. A strain refers to the stretching or tearing of muscle fibers or tendons. When it comes to the Achilles, these are typically graded:
- Grade 1 Strain: This is a mild strain involving microscopic tears in the tendon fibers. You might experience mild pain and tenderness in the Achilles area, particularly during or after activity. There's usually no significant loss of strength or range of motion, and you might be able to continue your activities with some discomfort.
- Grade 2 Strain: A moderate strain with more extensive tearing of the tendon fibers, though the tendon remains intact. Pain is more pronounced and persistent, often accompanied by swelling and bruising. You'll likely experience a noticeable reduction in strength and range of motion, making activities like running or jumping difficult or impossible. Walking might also be painful.
- Grade 3 Strain (Partial Rupture): This involves a significant tear through a large portion of the Achilles tendon, but some fibers remain connected. The pain is severe and immediate, often described as a sudden "pop" or "snap." Significant swelling, bruising, and a palpable gap in the tendon may be present. Weight-bearing is extremely painful, and you'll have considerable difficulty pushing off your foot.
- Achilles Tendon Rupture (Complete Rupture): This is the most severe Achilles injury, where the tendon completely tears, separating the calf muscles from the heel bone. The sensation is often described as being kicked or shot in the back of the ankle. There's intense, immediate pain, inability to push off the foot, and often a visible or palpable gap in the tendon. This injury typically requires surgical intervention to reattach the tendon.
Beyond acute strains, the Achilles tendon can also be affected by tendinopathy, a chronic condition characterized by pain, stiffness, and impaired function due to repetitive microtrauma and failed healing responses. This can manifest as Achilles tendinitis (inflammation) or Achilles tendinosis (degeneration of the tendon without significant inflammation). Both can lead to chronic pain and limit participation in activities if not addressed appropriately.
How Achilles Injuries Normally Occur: The Mechanics of Misfortune
Achilles injuries most commonly occur due to a sudden increase in load, repetitive stress, or inadequate preparation for activity. Understanding the typical movement patterns that lead to these injuries can help in prevention:
- Sudden, Powerful Push-Off: This is perhaps the most common mechanism for acute Achilles strains and ruptures. Think of sprinters exploding out of the blocks, basketball players jumping for a rebound, or tennis players pushing off to change direction rapidly. The Achilles tendon experiences immense tensile forces during these movements, and if the force exceeds its capacity, injury can occur.
- Sudden Dorsiflexion (Foot Flexed Upwards): While less common for ruptures, this can contribute to strains. If the foot is forcefully pulled upwards while the calf muscles are contracting, it can place excessive stress on the tendon.
- Repetitive Jumping or Running: Chronic overuse, particularly in activities involving repeated jumping (e.g., volleyball, basketball) or long-distance running, can lead to Achilles tendinopathy. The repetitive loading causes microscopic damage that the body struggles to repair, leading to inflammation and degeneration over time.
- Inadequate Warm-up: Skipping a proper warm-up leaves the muscles and tendons cold and less pliable, making them more susceptible to injury when suddenly subjected to high forces.
- Sudden Changes in Training Intensity or Volume: A rapid increase in the duration, intensity, or frequency of training can overload the Achilles tendon. For example, suddenly increasing mileage in running or adding more plyometric exercises without proper progression.
- Poor Biomechanics: Issues such as overpronation (feet rolling inward excessively), limited ankle dorsiflexion, or muscle imbalances in the lower limb can alter the mechanics of how force is transmitted through the Achilles, predisposing it to injury.
- Age and Degeneration: As we age, tendons naturally lose some of their elasticity and blood supply, making them more susceptible to injury.
- Certain Medications: Some medications, particularly fluoroquinolone antibiotics, have been linked to an increased risk of Achilles tendon rupture.
Best Ways to Load the Achilles Tendon: Strengthening for Resilience
Proper loading is key to both preventing Achilles injuries and rehabilitating them. It involves gradually increasing the stress on the tendon to stimulate adaptation and strengthen its structure. The principle of progressive overload is paramount here.
- Eccentric Loading: This is arguably the most critical component of Achilles tendon rehabilitation and strengthening. Eccentric exercises involve lengthening the calf muscles while they are contracting. Think of the lowering phase of a calf raise. Research consistently shows that eccentric training is highly effective in treating and preventing Achilles tendinopathy. This type of loading helps to remodel the tendon, increase its collagen synthesis, and improve its ability to withstand tensile forces.
- Examples: Eccentric calf raises (standing on the balls of your feet on a step, slowly lowering your heels below the step), single-leg eccentric calf raises.
- Heavy Slow Resistance (HSR) Training: This involves lifting heavier weights with slow, controlled movements. Unlike purely eccentric training, HSR engages both concentric and eccentric phases, promoting overall strength and hypertrophy of the calf muscles, which in turn supports the Achilles tendon.
- Examples: Weighted calf raises, leg press with a focus on calf engagement.
- Plyometric Progression: Once basic strength and pain-free movement are established, incorporating plyometrics helps to train the Achilles tendon's ability to store and release elastic energy. This prepares the tendon for the dynamic demands of sports and high-impact activities. Plyometrics should be introduced gradually, starting with low-impact drills and progressing to more demanding movements.
- Examples: Pogo hops, box jumps (low to high), jump rope, bounding.
- Gradual Return to Sport-Specific Activities: For athletes, the final stage of loading involves progressively reintroducing sport-specific movements. This could include controlled running drills, cutting, jumping, and agility exercises, mirroring the demands of their sport. This ensures the Achilles is adequately prepared for the unique stresses it will encounter during competition.
- Listen to Your Body: While progressive overload is essential, it's equally important to listen to your body and avoid overtraining. Tendon pain that worsens with activity or persists for more than 24 hours after a workout is a sign to back off and reassess your loading strategy. Rest and recovery are just as vital as training.
Benefits of Incorporating Plyometrics and the Stretch-Shortening Cycle
Plyometrics are exercises that involve rapid and powerful movements designed to improve power, speed, and elasticity. They are based on the principle of the stretch-shortening cycle (SSC), which is a natural mechanism in our muscles and tendons.
The SSC involves three phases:
- Eccentric (Stretching) Phase: The muscle is rapidly stretched, storing elastic energy in the tendon. Think of the loading phase before a jump – your muscles lengthen as you descend.
- Amortization (Transition) Phase: A brief, almost instantaneous pause between the eccentric and concentric phases. The shorter this phase, the more efficiently the stored energy can be utilized.
- Concentric (Shortening) Phase: The muscle rapidly shortens, releasing the stored elastic energy to produce a powerful movement. This is the "explosion" phase of a jump.
Incorporating plyometrics into your training offers numerous benefits, particularly for Achilles health and performance:
- Improved Tendon Elasticity and Stiffness: Plyometrics train the Achilles tendon to become more elastic and stiffer. A stiffer tendon can transmit force more efficiently, leading to more powerful movements and less energy expenditure. It also means the tendon can handle greater loads without deforming excessively.
- Enhanced Power and Speed: By optimizing the SSC, plyometrics enable muscles to produce more force in a shorter amount of time, translating to increased jumping height, sprinting speed, and overall athletic power.
- Increased Tendon Strength and Resilience: The rapid loading and unloading inherent in plyometrics stimulate adaptations within the tendon, making it stronger and more resilient to injury. It prepares the tendon for the high-impact forces encountered in sports.
- Improved Neuromuscular Control: Plyometrics enhance the communication between your brain and muscles, leading to better coordination, balance, and proprioception (your body's awareness in space). This can help with injury prevention by improving your ability to react to sudden changes in movement.
- Functional Training: Plyometric exercises often mimic movements found in sports, making them highly functional for athletes. They bridge the gap between basic strength training and the dynamic demands of competition.
However, plyometrics must be introduced gradually and with proper technique to avoid injury. Starting with low-impact drills and progressing to more intense movements is crucial, especially for individuals recovering from an Achilles injury.
How Performance Physical Therapy at Conquer Movement Can Help Prevent or Return from Injury
Conquer Movement's performance physical therapy approach is specifically designed to address the complexities of Achilles injuries, offering a comprehensive pathway for both prevention and rehabilitation. Our philosophy centers on not just treating the symptoms, but identifying and correcting the underlying biomechanical faults and strength deficits that contribute to these injuries.
For Injury Prevention:
- Thorough Biomechanical Assessment: We conduct a detailed analysis of your movement patterns, running gait, jumping mechanics, and lower limb alignment. This helps us identify subtle imbalances or inefficiencies that might be placing undue stress on your Achilles tendon.
- Strength and Mobility Screening: We assess the strength of your calf muscles, glutes, hamstrings, and core, as well as the mobility of your ankle, knee, and hip joints. Weakness or tightness in any of these areas can alter force transmission and increase Achilles vulnerability.
- Personalized Training Programs: Based on our assessment, we develop tailored strength and conditioning programs focusing on:
- Targeted Calf Strengthening: Emphasizing eccentric and heavy slow resistance training to build a robust Achilles tendon.
- Proximal Strength: Strengthening the glutes and core to improve stability and optimize lower limb mechanics.
- Ankle Mobility Drills: Ensuring adequate ankle dorsiflexion to reduce compensatory stress on the Achilles.
- Progressive Plyometrics: Safely introducing plyometric exercises to enhance tendon elasticity and power, preparing your body for the demands of your sport or activity.
- Movement Pattern Retraining: We provide expert coaching to refine your running, jumping, and landing mechanics, minimizing inefficient movements that could lead to injury.
- Education and Load Management Strategies: We empower you with the knowledge to understand your body, recognize early warning signs of overload, and implement effective training load management strategies to prevent overuse injuries.
For Returning from Injury:
- Accurate Diagnosis and Prognosis: Our physical therapists are experts in musculoskeletal injuries, providing an accurate diagnosis of your Achilles injury and establishing a clear prognosis for recovery.
- Individualized Rehabilitation Programs: Whether you've suffered a mild strain or a complete rupture (post-surgery), we design a phased rehabilitation program that progresses logically and safely. This includes:
- Pain and Swelling Management: Utilizing modalities and manual therapy techniques to reduce acute symptoms.
- Gradual Loading and Strengthening: Starting with gentle isometric exercises and progressively advancing to eccentric, heavy slow resistance, and finally, plyometric training as appropriate for your stage of healing.
- Range of Motion Restoration: Regaining full and pain-free ankle mobility.
- Proprioceptive Training: Re-establishing balance and joint position sense to prevent re-injury.
- Functional Progression and Sport-Specific Drills: Systematically reintroducing movements that mimic the demands of your sport or daily activities, building confidence and preparing your body for a full return.
- Manual Therapy and Soft Tissue Techniques: Our therapists utilize hands-on techniques to address tissue restrictions, improve circulation, and facilitate healing.
- Holistic Approach: We consider all factors influencing your recovery, including nutrition, sleep, and psychological readiness, ensuring a truly comprehensive rehabilitation experience.
- Minimizing Recurrence: Our ultimate goal is not just to get you back to your previous level of activity, but to make you stronger and more resilient than before, significantly reducing the risk of future Achilles injuries.
At Conquer Movement, we believe in empowering you to take control of your recovery and performance. By combining expert knowledge, individualized care, and a proactive approach, we help you not only overcome Achilles injuries but conquer your movement potential, ensuring a durable and vibrant active life. Don't let Achilles pain hold you back – let us help you move, perform, and live without limits. Call here to set up a discovery call!
Returning to sports and an active lifestyle also read:
- Mindset Shift from Injury to Return to Sport
- How Physical Therapy Keeps Wilmington Athletes Safe in Spring Sports
Dr. Evan Langley DPT, PT, CSCS
Performance Physical Therapist
Conquer Movement - Wilmington, NC
{% module_block module "widget_85b3e65b-b6b0-410d-ae04-8dea90a7ccd2" %}{% module_attribute "child_css" is_json="true" %}{% raw %}{}{% endraw %}{% end_module_attribute %}{% module_attribute "css" is_json="true" %}{% raw %}{}{% endraw %}{% end_module_attribute %}{% module_attribute "definition_id" is_json="true" %}{% raw %}null{% endraw %}{% end_module_attribute %}{% module_attribute "field_types" is_json="true" %}{% raw %}{"meeting":"meeting","select_meeting_description":"text","select_meeting_title":"text"}{% endraw %}{% end_module_attribute %}{% module_attribute "label" is_json="true" %}{% raw %}null{% endraw %}{% end_module_attribute %}{% module_attribute "meeting" is_json="true" %}{% raw %}"https://meetings.hubspot.com/steven-solecki"{% endraw %}{% end_module_attribute %}{% module_attribute "module_id" is_json="true" %}{% raw %}33947244299{% endraw %}{% end_module_attribute %}{% module_attribute "path" is_json="true" %}{% raw %}"@hubspot/meetings"{% endraw %}{% end_module_attribute %}{% module_attribute "schema_version" is_json="true" %}{% raw %}2{% endraw %}{% end_module_attribute %}{% module_attribute "smart_objects" is_json="true" %}{% raw %}[]{% endraw %}{% end_module_attribute %}{% module_attribute "smart_type" is_json="true" %}{% raw %}"NOT_SMART"{% endraw %}{% end_module_attribute %}{% module_attribute "tag" is_json="true" %}{% raw %}"module"{% endraw %}{% end_module_attribute %}{% module_attribute "type" is_json="true" %}{% raw %}"module"{% endraw %}{% end_module_attribute %}{% module_attribute "wrap_field_tag" is_json="true" %}{% raw %}"div"{% endraw %}{% end_module_attribute %}{% end_module_block %}

